We’ve all struggled with this at times. The hunt for ovaries. Pelvic exams can be quite frustrating when you know that there are only three organs in the pelvis, and you can’t find two of them!
Ovaries are tiny, surprisingly mobile and often hidden by bowel, so no wonder they test our skills and patience!
Ovaries are tiny, surprisingly mobile and often hidden by bowel, so no wonder they test our skills and patience!
Helpful plans of attack for finding ovaries:
1. Half-way empty the bladder.
Some bladders are just too full! You can usually tell when your female patient is writhing and grimacing.
Visually you can identify a too-full bladder by its rounded appearance and depth on screen exceeding 10 cm. That’s awfully far for your ultrasound beam to penetrate and those little ovaries will be squished into some tight corner of the pelvis. Off to the bathroom with her! Click here for tips on positively persuading her to partially empty!
Have your patient empty about halfway. A halfway (ish) full bladder gives you the belly flexibility to push a bit while you search and allows space in the pelvis for the ovary to return to view. Plus your patient will be so much happier and relaxed that you’ll both enjoy the scan much more.
Visually you can identify a too-full bladder by its rounded appearance and depth on screen exceeding 10 cm. That’s awfully far for your ultrasound beam to penetrate and those little ovaries will be squished into some tight corner of the pelvis. Off to the bathroom with her! Click here for tips on positively persuading her to partially empty!
Have your patient empty about halfway. A halfway (ish) full bladder gives you the belly flexibility to push a bit while you search and allows space in the pelvis for the ovary to return to view. Plus your patient will be so much happier and relaxed that you’ll both enjoy the scan much more.
2. Follow the ligaments.
Arising from the fundus of the uterus are the fallopian tubes, which lie wrapped in ligaments and vessels. Following these ligaments can often lead you right to an ovary. Ligaments are best seen when you are sweeping in transverse through the uterus, and can look like a tuft or pinched area arising from the lateral edges of the uterine fundus. Keep a close eye on them and carefully follow their wiggly path to the prized ovary!
Remember: the ovaries will never be further out laterally than the pelvic muscles, so be familiar with the striated appearance of muscle on ultrasound. And ovaries can often be surrounded by vessels so a scan with color Doppler on can sometimes outline the ovary nicely.
Remember: the ovaries will never be further out laterally than the pelvic muscles, so be familiar with the striated appearance of muscle on ultrasound. And ovaries can often be surrounded by vessels so a scan with color Doppler on can sometimes outline the ovary nicely.
3. Thorough attentive sweeps.
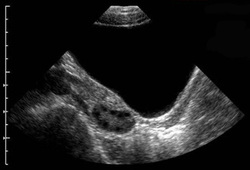
Expect to make many overlapping sweeps through the pelvis while on the search for ovaries. Begin in the midline where you assess the uterus and then work your way out laterally bit by bit always using the bladder as a window. Always sweep and search in both transverse and sagittal views. Sometimes that little ovary pops out at just a certain angle.
And be attentive for the ovary sign. That is what I call the little “blip” you see when you sweep past something small, oval and discrete amongst all the windy vessels and shadowy bowels in the pelvis.
And be attentive for the ovary sign. That is what I call the little “blip” you see when you sweep past something small, oval and discrete amongst all the windy vessels and shadowy bowels in the pelvis.
4. Check the Greater Pelvis.
The Greater or False Pelvis extends up to the top of the hip bones, almost to the navel. The Lesser or True pelvis is quite a small area very low down in what I consider to be the teeny-tiny-bikini area. After assessing the True pelvis thoroughly for ovaries I always make a few sweeps up towards the navel and assess both the left and right lower quadrants (LLQ & RLQ). Sometimes the ovary has migrated up there and can be found lounging about quite superficially.
Important: If your patient has any type of pain in the LLQ or RLQ always thoroughly assess those areas. It could be a sign that an ovary is up there (with a possible pathology that is causing the pain).
Important: If your patient has any type of pain in the LLQ or RLQ always thoroughly assess those areas. It could be a sign that an ovary is up there (with a possible pathology that is causing the pain).
5. Had any pelvic surgery?
If I’ve completed a thorough assessment of both the Lesser and Greater pelvis and still not seen an ovary, I’ll ask if she’s had any pelvic surgeries.
These days the scars from laparoscopic surgeries are so tiny that you’ll never see them, so clear questioning is best.
Although complete removal of an ovary is rare, it does happen with some complex cyst or dermoid removals. You just don’t know, so always ask. That way you won’t be wasting your time searching for something that may not even be there.
These days the scars from laparoscopic surgeries are so tiny that you’ll never see them, so clear questioning is best.
Although complete removal of an ovary is rare, it does happen with some complex cyst or dermoid removals. You just don’t know, so always ask. That way you won’t be wasting your time searching for something that may not even be there.
6. Do an EV.
If she definitely has both of her ovaries but you’ve had no luck seeing them trans-abdominally, it’s time to do an endovaginal scan.
Once you’re all set up, start again in the pelvic midline and sweep your way out laterally from the uterus until you see a glimpse of the ovary. The real key to EV scans is to use firm pressure to move the bowel gas out of the way, but to apply it very slowly and evenly. No jerking around in there, it’s a sensitive place. Always keep your transducer movements slow and gentle.
You can also have the patient help you out a bit by using both her hands to push slowly and firmly down on her pelvis to help push the ovary into your field of view and move aside some of the bowel gas. Some patients actually like being able to help out a bit.
Another little trick: When assessing the right side of the pelvis with EV, reverse the transducer orientation (turn it around in your hand and hold it backwards) and push the Reverse Image button. When you reverse both the transducer and the image you get the correctly aligned orientation on the screen. This allows you to take advantage of the small angle of the transducer head to see further into the right adnexa. (This takes a bit of practice but is very useful.)
Once you’re all set up, start again in the pelvic midline and sweep your way out laterally from the uterus until you see a glimpse of the ovary. The real key to EV scans is to use firm pressure to move the bowel gas out of the way, but to apply it very slowly and evenly. No jerking around in there, it’s a sensitive place. Always keep your transducer movements slow and gentle.
You can also have the patient help you out a bit by using both her hands to push slowly and firmly down on her pelvis to help push the ovary into your field of view and move aside some of the bowel gas. Some patients actually like being able to help out a bit.
Another little trick: When assessing the right side of the pelvis with EV, reverse the transducer orientation (turn it around in your hand and hold it backwards) and push the Reverse Image button. When you reverse both the transducer and the image you get the correctly aligned orientation on the screen. This allows you to take advantage of the small angle of the transducer head to see further into the right adnexa. (This takes a bit of practice but is very useful.)
So there are my 6-Hard-Earned-Ovary-Hunting-Strategies. Some days I have to use them all! But going through all the steps allows me the confidence of knowing that I did everything possible to thoroughly assess that pelvis and help my patient.
Happy Scanning!
Do you have any other Ovary-Hunting-Strategies that you use? Share them in the comments below, I’d love to hear them!
Happy Scanning!
Do you have any other Ovary-Hunting-Strategies that you use? Share them in the comments below, I’d love to hear them!